A Study Guide for the Chronically Ill: 23 Proven Strategies

Walker Payne is a Type 1 Diabetic and Data Scientist at Gluroo. There, he helps develop an app for collaborative diabetes management that empowers families and individuals to worry about diabetes less, and live life more. Gluroo is a powerful tool built for all T1D journeys and can be downloaded for free today on both Android and iOS.
I’ve been a Type 1 Diabetic for over 14 years, or about half my life. In that time, my views and knowledge of the disease have changed dramatically.
At the age of 13, when I was diagnosed, I was like many other pubescent kids; I really didn’t care. I didn’t appreciate the disease for what it was, I didn’t know anything about clinical guidance or A1C scores, and I tried my best to hide the fact that I had it. All I really wanted (understandably) was to forget about it and to put in the bare minimum effort required to live a relatively normal life with few complications. Anything more was asking too much.
Fast forward to now. I’m 27 years old and a Data Scientist at a healthtech startup. I maintain a Time in Range (TIR) of over 90% on average – meaning my blood glucose is within the “normal” range over 90% of the time, comparable to a non-diabetic. I also have consistent HbA1C scores (a blood test that measures your average blood glucose levels over the past 2-3 months) around 5.5%. I’m privileged in that it is quite literally my job to understand this disease and to analyze patterns in blood glucose data on a daily basis.
My goal for this post is to provide some quick, actionable pieces of advice that I wish I had known from the beginning. I’m hoping to distill down these 14 years of personal and professional experience with the disease into tactical wisdom that you can use to live a happier, healthier, and complication-free life as a T1D. Without further ado, let’s get into it.

I read a book a few years ago about building successful businesses called ‘Good to Great’ by Jim Collins. One of the common rules he identifies among leaders of great companies is that they are hyper aware of the truth of their situation. He argues that in order to find the path to greatness, you must first “confront the brutal facts of your current reality.”
He expands:
“When you start with an honest and diligent effort to determine the truth of your situation, the right decisions often become self-evident. It is impossible to make good decisions without infusing the entire process with an honest confrontation of the brutal facts.”
This is something that I’ve tried to keep in mind with regards to diabetes management. Diabetes can be a brutal, terrible disease. It has a plethora of complications that can manifest as a result of poor management. It’s easy to want to look away, to shield yourself, from the mental burden of fully acknowledging these horrors. I believe, however, that it’s important to understand these very real and very scary complications. Consider it an exercise in Stoicism, a chance to face the challenges of life and surmount them.
So with that said, join me as we briefly discuss some of the downsides of poor glycemic control. As a Type 1 Diabetic, it’s your job to understand these so that you can fully appreciate the importance of your work.
What follows are a handful of complications that can arise due to poor glycemic control:
The list goes on and on – these are just a few of the complications that I hand-picked from the previous Mayo Clinic link. According to the Cleveland Clinic, “close to 50% of people with Type 1 diabetes will develop a serious complication over their lifetime”.
Yes, I’m intentionally picking statistics and facts in a “scared-straight” manner. The point to get across is that T1D complications are comprehensive, frightening, and very, very real.
But now that we’re aware of the downsides, let’s go back to the second part of rule #1 – never lose hope. This is the most important part of diabetes management by far. We have to understand that it is entirely possible to live a happy, healthy, and complication-free life as a T1D:
Conventional wisdom these days supports striving for an HbA1c score of less than 7%. HbA1c is a lab-derived measure of your average blood glucose levels over the last 2-3 months. A target of 7% corresponds to a BGL of ~154 mg/dL or 8.6 mmol/L. (For context, a non-diabetic may spend roughly 90% of their day in the range of 70 to 120 mg/dL.) This was shown to significantly reduce the risk of developing nearly all T1D complications, in some cases by up to ~75%.
Further hope can be derived from the fact that there are thousands, if not hundreds of thousands, of Type 1 Diabetics living with an HbA1C score of less than 7%.
There’s no reason why this trend of technological advancement, knowledge, and education about the disease shouldn’t continue to improve over time. Another way of phrasing this is that for every day that goes by, your odds of living longer as a T1D increase.
Knowing this makes me extremely hopeful for my future and your future. Today is the best time in history to be a Type 1 Diabetic, so let’s take advantage of the tools we have at our disposal to live a better life.
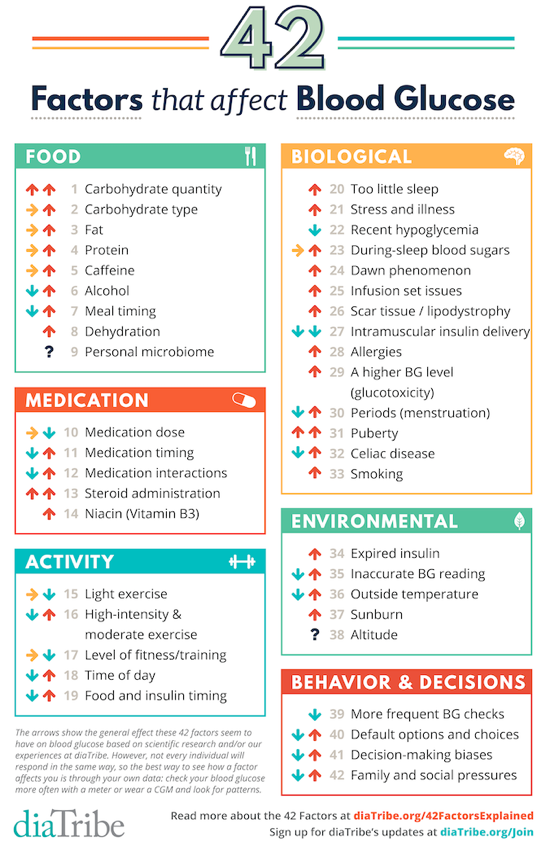
Speaking of tools at our disposal, the next life hack for managing T1D is to get a continuous glucose monitor. Studies have shown that CGM use helps patients to significantly reduce HbA1C scores and to prevent hypoglycemia more effectively. The fact of the matter is that it’s nearly impossible to understand the full suite of factors that affect blood glucose levels (see image above) without constantly wearing a CGM.
It’s hard to find a good figure, but sources like the T1DExchange indicate that from 2016-2018, only 27% of T1D patients were using a CGM. I believe that every T1D would benefit from having a CGM and I wish I could wave a magic wand and make it so.
Unfortunately, CGMs are still pretty expensive and not everyone has the same level of access to them. The good news is that you may be able to get a free sample to at least get a taste of what they can do for you. Even 10 days of wearing a CGM will be massively beneficial to your understanding of this disease and how various things you do affect your BGL (Blood Glucose Level).
Here are some links to forms you can fill out to request a free CGM sample (in the US):
Wearing a CGM will help you develop your own highly-personalized tricks of management. For example, I know that I can go for a 10-15 minute walk after any meal and activate my insulin more quickly than if I were to sit at my desk. It’s one thing to read about this effect, but it’s even more persuasive when you see it first hand with your own data.
The last tip I’ll share today is related to wearing a continuous glucose monitor (CGM) at all times: log everything you do – including carbohydrate consumption, insulin doses, and exercise – for at least two weeks!
Logging your meals, insulin and activities is important because it’s the only way to identify patterns in your BGL – both good patterns and bad. This, combined with a CGM providing BGL readings every 5 minutes, is the most powerful exercise at your disposal for truly understanding the ups and downs of blood glucose management.
When you start, it may feel overwhelming and mentally taxing. That’s totally normal. You can do it though, especially for just two weeks – it doesn’t have to be the rest of your life. The things you’ll learn about your own body and how it responds to various types of meals, insulin dose sizes, and other habits will be astounding.
My previous example of post-meal walks reducing BGL becomes incredibly clear only once you start to annotate the fact that you took a walk. It’s much harder to infer trends in your data from memory, and much easier if you have a log of those types of activities to look back on.
You can also log things like going out to your favorite restaurant to learn the best way to manage your BGL after a special meal. The next time you visit that place, you can just search in your history or scroll back in time to when you went there last, see how much you ate, how much insulin you dosed, and your resultant BGL, and modify your behavior accordingly.

There are some really powerful tools out there that help you keep track of exercise and overall health. MyFitnessPal is awesome for keeping track of meal macros (protein, fats, and carbs), calorie intake, and exercise. If you don’t have a CGM, mySugr makes your blood sugar readings from a finger-prick test much more useful, especially if you log your meals as well.
Again, I’m not saying you have to log every meal macro and exercise for the rest of your life. Just try it for a few weeks and see how it feels. You’ll learn so much along the way that you might decide it’s worth the hassle.
At the end of this two week period, you’ll have built a valuable database of meal examples that you can look back on in the future. You’ll understand exactly where you stand in terms of Time in Range (TIR) and GMI (an estimate of HbA1C), which will help you decide how aggressively to work in the future to maintain or improve them.
And the most important benefit of all is that the lessons you learn from two weeks of experimentation can stick with you for the rest of your life, allowing incremental changes in your diabetes management to have profound long-term effects on your overall health and wellness.

My journey as a Type 1 Diabetic has taken me from a place of ignorance and indifference to one of knowledge and empowerment. I’ve learned that confronting the harsh realities of this disease is essential, but it should never extinguish the flame of hope. Diabetes comes with a laundry list of potential complications, but the good news is that we’re living in an era of progress, where technology and research continue to improve our prospects.
Three key takeaways from this post:
Remember, you have the tools and knowledge at your disposal to lead a fulfilling life with T1D. Embrace the present moment, continue to learn, and use these insights to thrive in your journey with diabetes.
Diabetic and minding your food intake? Learn more about how you can stick to any kind of medical diet that’s best suited for your personal situation, and what you can do to curb your cravings.